Rural New Mexico Patients Deserve the Right. Surprise Medical Billing Solution
/For patients in New Mexico and nationwide, surprise medical billing is an issue that impacts their ability to afford the high-quality, comprehensive care they need. Often, these unexpected costs arise after an emergency situation in which the patient may not even know the treatments they are receiving would not be covered by their insurance plans.
New Mexico legislators have passed a law protecting patients from surprise medical bills, but even that does not cover roughly a third of patients. That is why Congress must make federal legislation to end surprise medical billing a priority.
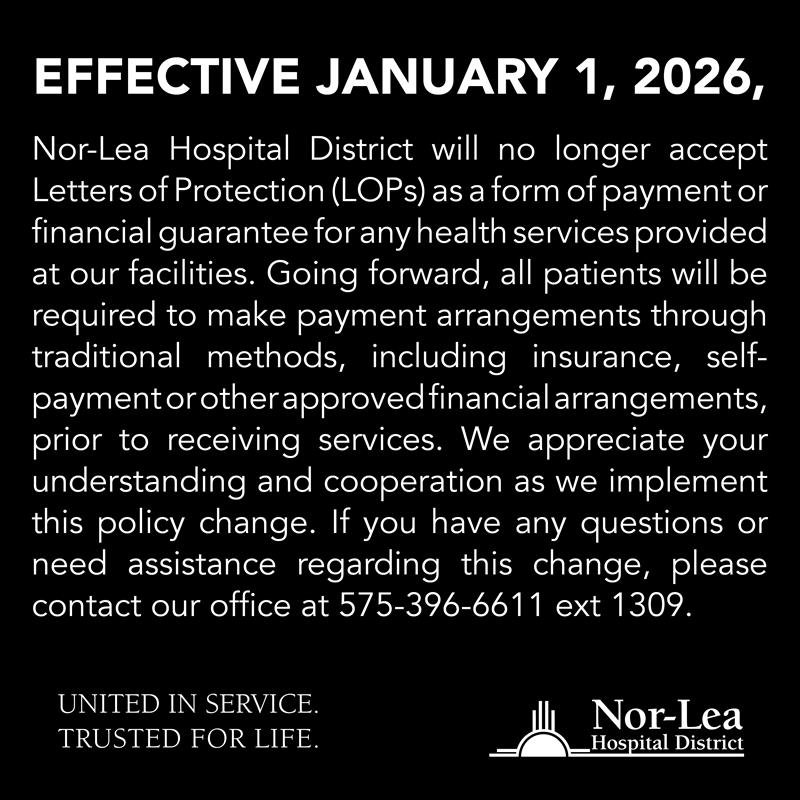
At Nor-Lea Hospital, which serves rural communities in southeastern New Mexico, we make every effort to mediate surprise bills on behalf of our patients to ensure the best possible patient experience. After all, many of the patients we treat day in and day out are our friends and neighbors. However, not all hospitals across the state and the country are able to take these extra steps on behalf of patients, further underscoring the need for congressional action.
However, as Congress closes in on a solution for surprise medical billing, it is vitally important that whatever bill they pass does not unintentionally threaten access to health care or affordability for any patients—particularly those living in rural communities where both of these factors already act as barriers to care. That means Congress must avoid any purported solutions that rely on a government benchmarking approach to ending surprise medical billing.
Under a benchmarking model, the government would set out-of-network rates for physicians using insurance companies’ in-network averages. However, because these in-network rates often include deep discounts that arise during contract negotiations, that means physicians would see their insurance reimbursements drop dramatically. These losses would be passed onto local hospitals and emergency rooms, many of which—especially in rural areas—are struggling as it is.
Such an approach could further undermine rural health care by contributing to already high rates of provider consolidation and exacerbating a growing physician shortage that is sweeping the nation. Patients in rural communities already have to travel longer distances and face longer waiting times to get the care they need; benchmarking could make these factors much worse while also driving up costs.